When Hives Won't Go Away

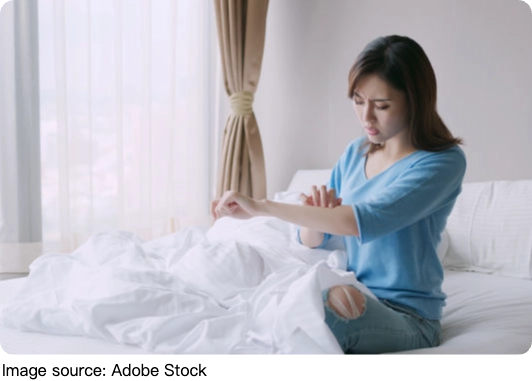
Hives, medically known as urticaria, are common skin reactions characterized by itchy, red, swollen welts.
While many people experience hives as a brief episode triggered by allergies or stress, a subset suffers from chronic hives—persistent outbreaks lasting more than six weeks.
This condition, often frustrating and complex, demands a nuanced approach to diagnosis and treatment.
What Are Chronic Hives?
Chronic hives, or chronic spontaneous urticaria (CSU), affect approximately 1.4% of the population, disproportionately impacting women twice as often as men. Unlike acute hives, which have identifiable triggers such as foods, medications, or infections, chronic hives often appear without a clear external cause. The welts typically come and go unpredictably, lasting from months to even several years in some cases.
Dr. Farheen Mirza, an allergist, explains that over 90% of chronic hives cases have no identifiable trigger, making them particularly challenging to manage. Some cases may be linked to autoimmune disorders, where the immune system mistakenly attacks the body's own tissues, or associated with thyroid and hormonal imbalances. However, the majority remain idiopathic, meaning their exact cause remains unknown.
Diagnosing Chronic Hives: Beyond the Surface
Diagnosis begins with a thorough clinical evaluation. Physicians look for hallmark signs: raised, itchy bumps that blanch when pressed and typically last less than 24 hours before fading. Keeping a detailed symptom diary is often recommended, tracking factors such as diet, medications, environmental exposures, and stress levels to identify potential triggers.
Blood tests may be ordered to rule out underlying autoimmune or thyroid diseases. In rare cases, a skin biopsy might be performed to exclude other dermatological conditions. Accurate diagnosis is critical, as it guides the treatment strategy and helps avoid unnecessary interventions.
Treatment Strategies: Tailored and Progressive
Managing chronic hives requires a personalized, step-wise approach. Initial treatment usually involves nonprescription antihistamines such as loratadine (Claritin) or fexofenadine (Allegra). If standard doses are insufficient, clinicians may increase antihistamine dosages under medical supervision.
For patients unresponsive to antihistamines alone, additional medications can be introduced. These include ranitidine (traditionally used for heartburn), montelukast (an asthma medication), and doxepin, which has antihistamine properties. In more severe or refractory cases, biologic therapy with omalizumab (Xolair) — a monoclonal antibody that targets IgE has demonstrated significant efficacy and safety in clinical studies.
Managing Expectations and Quality of Life
Chronic hives can severely impact daily life, causing intense itching, sleep disturbances, and emotional distress. Patients often report difficulty concentrating and lowered self-esteem due to visible skin lesions. Experts emphasize the importance of setting realistic expectations.
Improvement may take weeks or months, and treatment often involves trial and error to find the most effective regimen. Maintaining optimism and working closely with an allergist or dermatologist can significantly improve outcomes.
Dr. Emily Lawson, a leading dermatologist specializing in chronic skin conditions, highlights the evolving understanding of CSU, "While the precise cause of chronic hives remains unclear for many patients, advances in immunology have dramatically improved treatment options. Biologics like omalizumab have transformed care, providing new hope for those who previously had limited relief."
Chronic hives present a complex medical challenge due to their unpredictable nature and often unknown triggers. However, with a comprehensive diagnostic approach and a personalized, stepwise treatment plan including modern biologic therapies—most patients can achieve meaningful symptom control.
Collaboration between patients and healthcare providers, combined with realistic expectations and supportive care, is key to restoring quality of life for those affected by this persistent condition.
-
 Bogotá Travel MagicThis Magical Mountain City Has Views, Gold, and a Wild Restaurant Party!
Bogotá Travel MagicThis Magical Mountain City Has Views, Gold, and a Wild Restaurant Party! -
 Bacteria: Friend or Foe?Are Bacteria Our Friends or Enemies? Understanding Their Role in Health and Daily Life
Bacteria: Friend or Foe?Are Bacteria Our Friends or Enemies? Understanding Their Role in Health and Daily Life -
 Top Acne Fixes You Need!Struggling With Breakouts? Find Out Which Skincare Heroes Calm Redness Fast!
Top Acne Fixes You Need!Struggling With Breakouts? Find Out Which Skincare Heroes Calm Redness Fast!